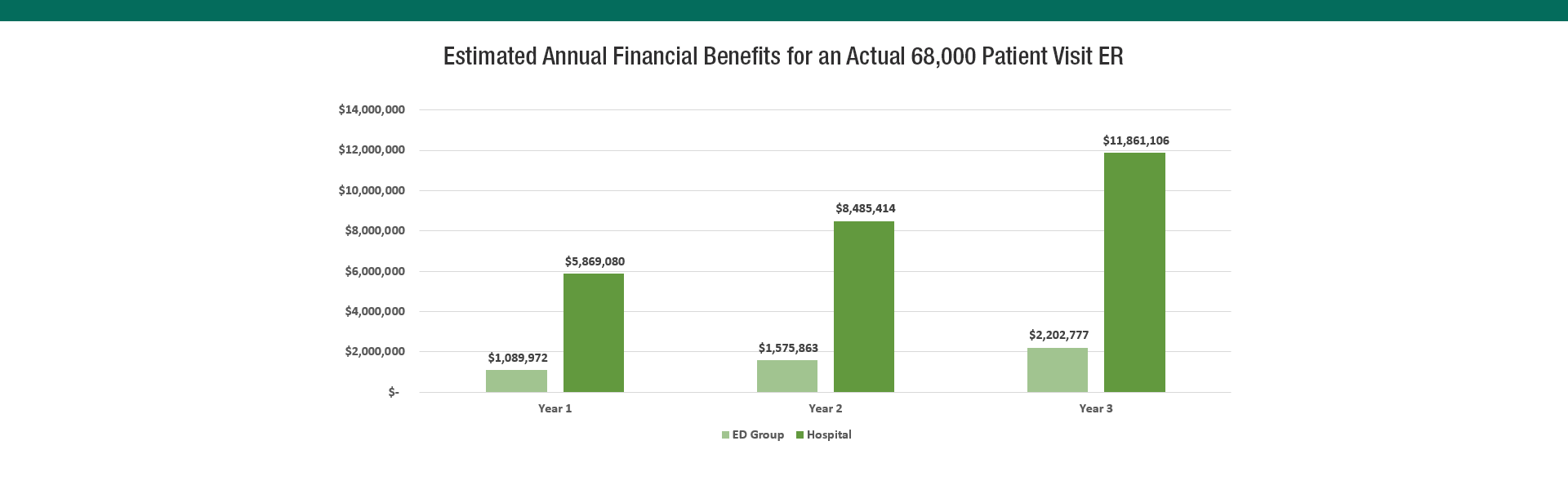
$31 Million in Financial benefits in 3 years
The numbers presented are not theoretical. They are actual 3-year financials for a real 68,000 patient visit emergency department. In the third year, the combined benefit for group and hospital was $167 PPV ($26 PPV for the group and $141 PPV for the hospital). Of course your group and or hospital may vary.
By every financial measure, Carepacity’s smart assignment system has been proven to show a positive return on investment (ROI). The attached spreadsheet looks at both a 12 month ramp and 10 year scenario.
Key Metrics for the model include:
- Annual patient visits
- Current average LWBS / LBTC
- Baseline growth rate
- Average collected ED group revenue PPV
- Average collected Hospital revenue PPV
- Average collected Hospital revenue PPV
- Annual Nurse Turnover Rate
Recapture LBTC Revenue
Recapturing Left without being seen (LWBS) and or Left Before Treatment Complete (LBTC) revenue is typically an immediate benefit of the system. For a 60,000 PV group, each 1% represents 600 visits. That translates to $90,000 for the group and $270,000 for the hospital.
In our actual case study, the emergency room dropped LWBS from 3% to near zero and recovered a nearly $300K ($4 PPV) for the group and over $1 million ($14 PPV) for the hospital.
This would typically more than justify the investment in the Carepacity service.
Increase in Emergency Room Patient Volume
Our case study emergency room saw a sizable bump in patient volume over a 2% baseline growth rate. The first year year to year increase was 11% or 9% over baseline. This translated to additional 6120 annual visits, nearly $800K in ED Group and $2.7 million in Hospital revenue.
Additional Hospital Admission Revenue
The Emergency Room is a front door for admissions to the hospital. General hospital admission rates can run around 20%. Most of these will be higher acuity ( ESI 1s and 2s). We assumed 10% of the additional patient volume would eventually be admitted. This is not an unreasonable assumption given that the increase in ER volume came from both reducing LBTC and new growth. Assuming a $2500 average collected revenue per patient ( $10,000 X 25% collection rate) we estimate the hospital brought in an additional $2 million in the first year, $3 million in the second and $4.2 in the third.
Reduced Physician and Staff Turnover
Due to fairly unusual circumstances, provider turnover wasn’t an issue in our case study but is an issue at many departments and hospitals. In fact, a Stanford study estimates that it might cost nearly a quarter million dollars to recruit and place a physician. Our model includes cells for number of staffed nurses, current turnover rates and reduction in turnover assumptions. A 50% reduction in a 10% annual turnover rate might reduce nurse recruitment costs by around $250 K.
Other Intangible and Reputational Benefits
A few years ago, a toddler named Malyia Jeffers had her feet and hands amputated because of a 5 hour wait in the emergency room. Essentially, she was triaged incorrectly by the nurse on duty. This tragedy ended in a $10 million settlement. Had this hospital been using smart assignment, Malyia would most likely have been seen in minutes and the physician would have discovered Malyia was in fact suffering from Bacterial Meningitis. The settlement was $10 million but the reputational damage to the hospital was probably much greater.
